The Hidden Threat: A Man’s Battle with Metastatic Melanoma of Unknown Primary
A Mysterious Beginning
It started as a small lump—barely noticeable—on the upper chest of a 73-year-old man. He dismissed it at first. After all, he had never smoked, rarely drank, and had only a few minor health problems in his lifetime. The lump, however, had other plans.
Over the course of a year, it grew. Slowly at first, then more rapidly. By the time he sought medical attention, the mass had become necrotic, oozing fluid and blood, and had expanded to 20 centimeters. What had once been a minor concern was now impossible to ignore.

His family had started to worry. He was more fatigued than usual, short of breath, and even his voice sounded different. A trip to the emergency department would mark the beginning of a journey neither he—nor his loved ones—expected.
An Unexpected Diagnosis
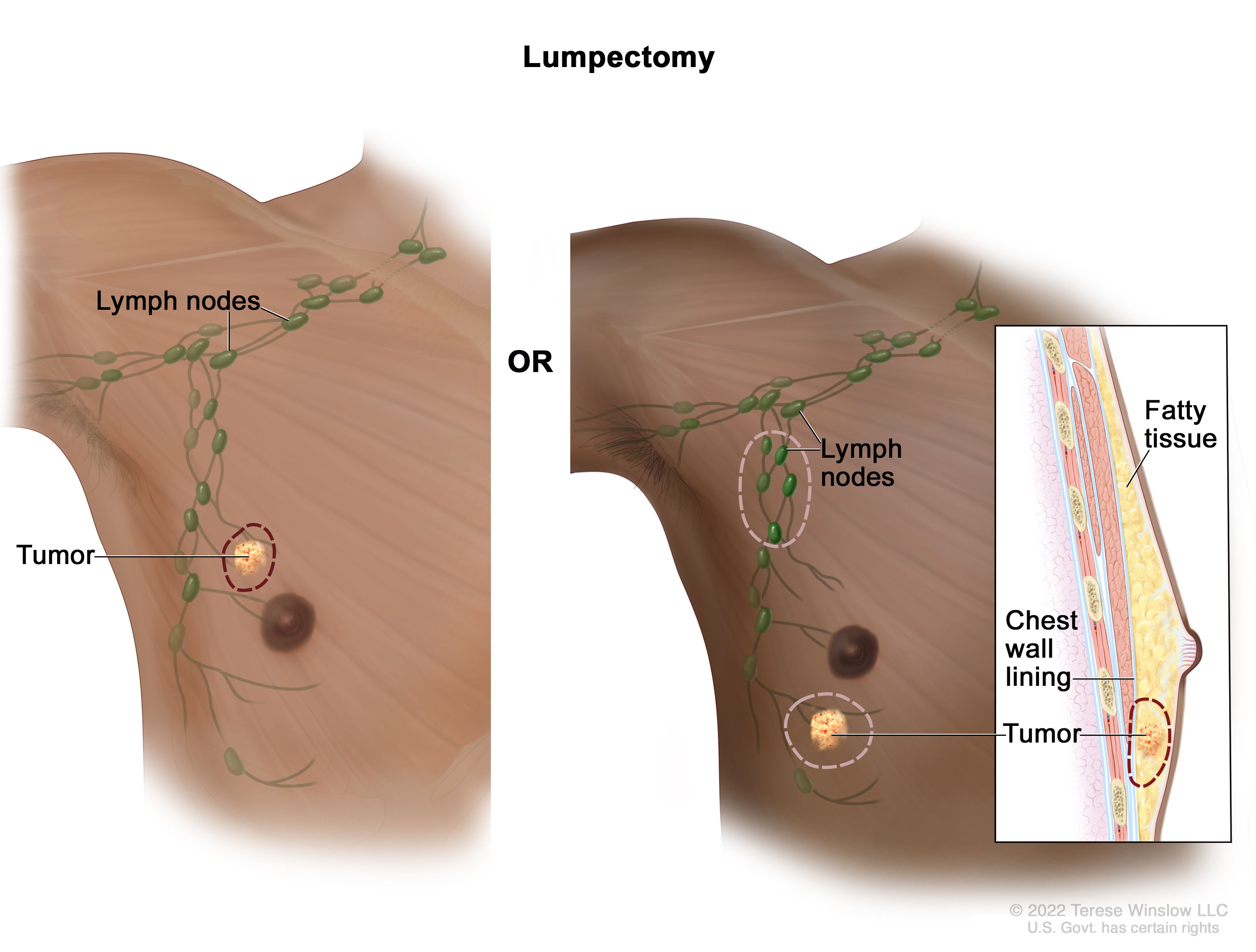
Doctors immediately ordered imaging tests. A CT scan revealed a large mass on his chest wall near his axilla (underarm), along with enlarged lymph nodes. The findings raised red flags. Surgery was scheduled to remove the tumor and ease his symptoms. However, surgeons couldn’t fully remove the mass due to its involvement with nearby nerves.
When the pathology results came back, they confirmed a surprising diagnosis: metastatic melanoma. But here’s what puzzled doctors most—there was no visible primary tumor on his skin, eyes, or mucosal tissue. After thorough examinations and imaging, no source could be found. He was diagnosed with metastatic melanoma of unknown primary (MUP), a rare and often misunderstood condition.
What Is Melanoma of Unknown Primary?
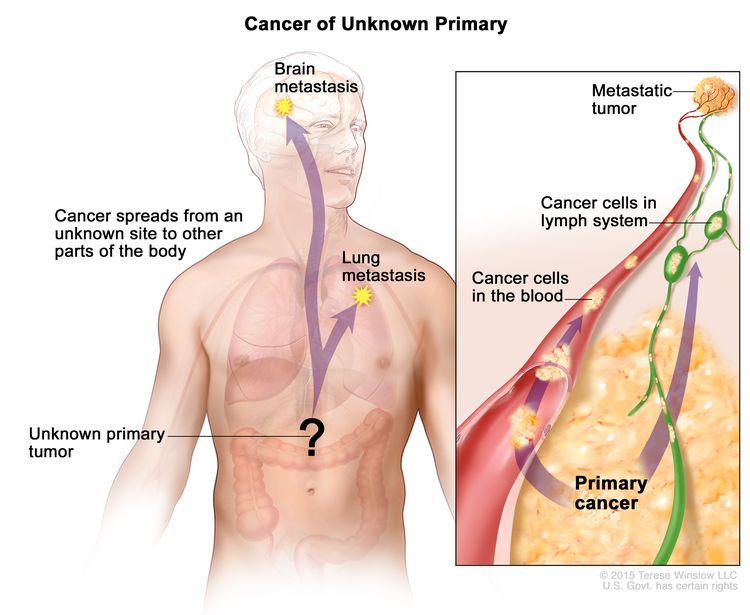
Melanoma is an aggressive form of skin cancer originating from melanocytes, the pigment-producing cells in the body. Typically, melanoma begins on the skin and spreads to lymph nodes or organs. But in the case of MUP, patients have no identifiable original tumor.
First described in the 1950s, MUP accounts for about 1% to 8% of all melanoma cases. Its cause is still under debate. Some theories suggest the original lesion may have regressed on its own—disappearing before detection—while others believe it may have been misdiagnosed or removed without biopsy.
To officially diagnose MUP, doctors must rule out several possibilities: incomplete physical examinations, removal of lesions without histological review, or atypical presentations in organs like the eyes or genitals.
The Personal Impact

The patient and his family were in shock. He had never shown signs of skin cancer. The family history was limited to lung cancer in his sister—nothing that seemed connected. He began to reflect on what he had missed. Could he have done something differently? Should he have gone to the doctor sooner?
More importantly, how could he—and others—have recognized the signs of something so silent, yet so aggressive?
Risk Factors and Hidden Dangers

Unlike typical melanoma, MUP has no definitive risk profile. It does tend to occur more often in men and typically appears in those between 40 and 60 years old. Fair-skinned individuals, those with extensive sun exposure, or a family history of melanoma may be at greater risk. But in many cases—including this one—none of those applied.
The most widely accepted explanation for MUP is spontaneous regression. Melanoma is one of the few cancers that can sometimes disappear on its own due to the body’s immune response. However, this means it can still spread elsewhere—leaving behind no trace of its origin.
Staging and Treatment Options
Because the patient’s disease was found in his lymph nodes and chest wall, without a primary lesion, it was classified as stage III metastatic melanoma. If his organs had been involved, the classification would have escalated to stage IV.
Treatment typically includes a combination of:
- Surgery: To remove large masses or affected lymph nodes.
- Radiation therapy: Used post-surgery to control local spread.
- Immunotherapy: Targeting specific pathways that melanoma cells use to evade the immune system.
In this case, the man underwent surgery followed by immunotherapy and localized radiation. His tumor load decreased, and surrounding lymph nodes began to show signs of regression—a hopeful sign.
Advances in Therapy
New treatments have significantly improved outcomes in melanoma. Two major approaches include:
- Checkpoint inhibitors: Drugs like nivolumab and ipilimumab help the immune system detect and destroy cancer cells.
- Targeted therapy: For tumors with mutations in genes like BRAF or ALK, medications can block these mutations and slow tumor growth.
Our patient tested positive for mutations in BRAF V600E and ALK R557C, allowing doctors to use targeted therapies tailored to his tumor’s biology. These advances have brought renewed hope to patients who once had limited options.
What We Can Learn
Melanoma of unknown primary remains a diagnostic and emotional challenge. It presents silently, often with vague symptoms or a single swelling that grows over time. It can affect those who live healthy lives and have minimal risk factors.
The key takeaway?
- Don’t ignore unusual changes in your body. A persistent lump, a draining wound, or unexplained fatigue should never be brushed aside.
- Early imaging and biopsy save lives. If detected early, aggressive melanoma—even in rare forms like MUP—can be treated more effectively.
- Stay proactive. Annual check-ups and skin evaluations remain crucial, even if you believe you’re low-risk.
A Story of Resilience
This man’s journey isn’t just about a rare medical condition. It’s a testament to resilience—of seeking help, enduring surgery, and navigating months of therapy with courage. With his care team’s support and the love of his family, he’s now in recovery, focused on healing and spreading awareness.
His case reminds us that cancer doesn’t always follow a clear script. Sometimes, it’s the unknown that challenges us most. But with the right care, early detection, and modern medicine, even the most mysterious diagnoses can be met with hope.
Sources:
- American Cancer Society – Melanoma Overview
- National Cancer Institute – Melanoma of Unknown Primary
- DermNet – Metastatic Melanoma
- PubMed – ALK mutations in melanoma
Note: This article is for educational purposes and should not replace professional medical advice.



